The Ancient Protein Clock That Ticks Without DNA

TL;DR: Scientists are reversing immune aging by regenerating the thymus - a critical organ that trains T-cells but shrinks with age. Clinical trials show hormone therapies can restore thymic function and even reverse biological age markers, with treatments potentially available within a decade.
By 2040, scientists predict that thymus regeneration could become as routine as a vaccine booster - a simple intervention that restores your immune system to its youthful peak. What's happening in laboratories right now isn't just extending lifespan. It's fundamentally reimagining what it means to age.
Your immune system has a master control center, a small butterfly-shaped organ tucked behind your breastbone. The thymus trains T-cells, those cellular warriors that identify and destroy everything from flu viruses to cancer cells. Here's the catch: your thymus starts dying when you're still a teenager.
By age 50, most people have lost about 75% of their thymic tissue. By 70, it's nearly gone. This isn't just an anatomical curiosity - it's why elderly people die from infections that wouldn't faze a 20-year-old, why vaccines work less effectively with age, and why cancer rates skyrocket after 65.
But researchers have identified a pattern that immunologists never predicted: the thymus doesn't want to die. Given the right molecular signals, it can rebuild itself.
In 2019, a small clinical trial at Stanford University did something unprecedented. Nine healthy volunteers between ages 51 and 65 took a cocktail of three drugs: growth hormone, metformin, and DHEA. The goal was modest - see if they could slow thymic decline.
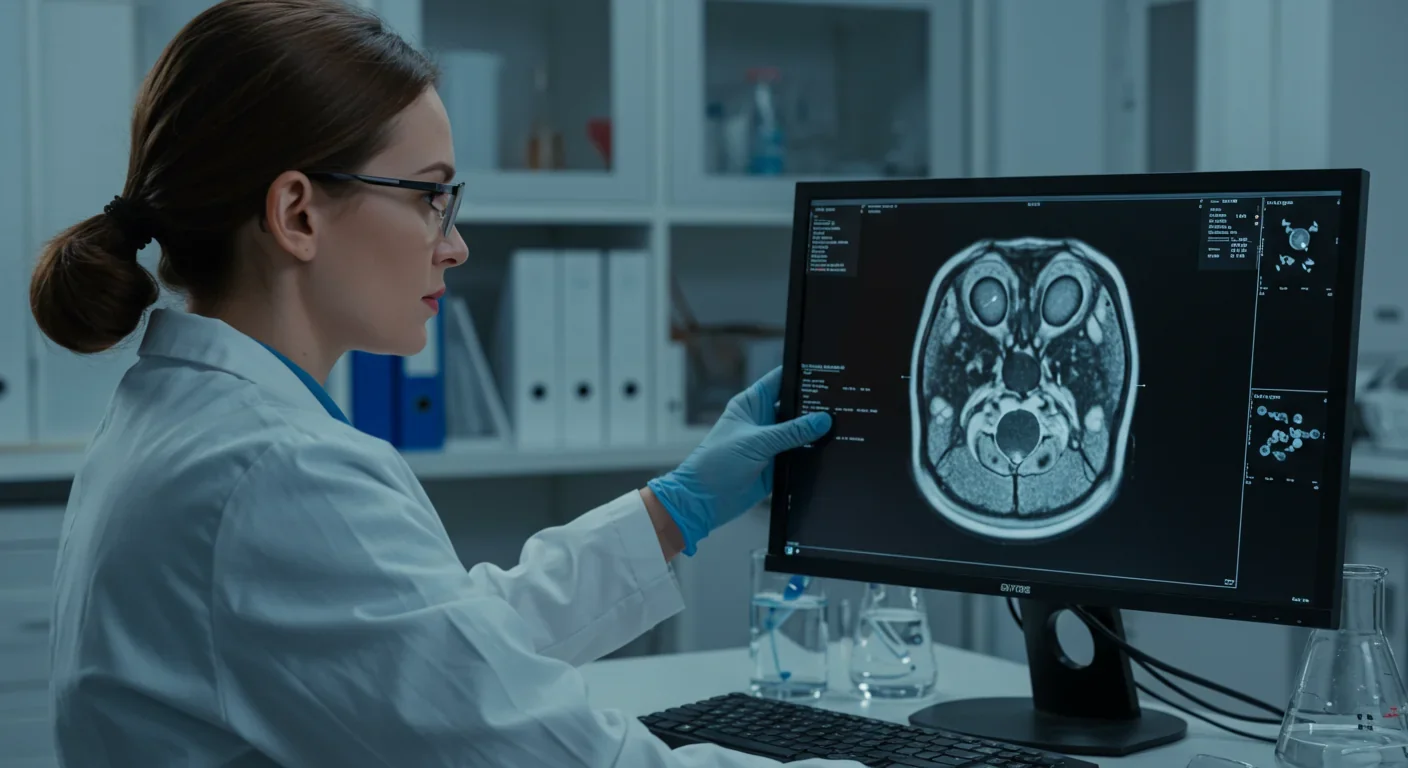
What happened instead shocked the researchers. MRI scans showed that participants' thymuses had actually regenerated, replacing fatty tissue with functional thymic cells. Even more remarkable, their epigenetic clocks - molecular markers of biological age - reversed by an average of 2.5 years.
This wasn't just slowing aging. This was reversing it.
The trial, known as TRIIM (Thymus Regeneration, Immunorestoration, and Insulin Mitigation), represented the first time scientists had demonstrated actual thymic regrowth in humans. The results were so unexpected that lead researcher Gregory Fahy initially thought there must have been a mistake in the imaging.
There wasn't. Follow-up studies confirmed the finding, and now a larger trial called TRIIM-X is underway with 80 participants aged 40-80, aiming to validate these results and understand the mechanisms behind them.
To grasp why this matters, you need to understand what the thymus actually does. Think of it as a boot camp for your immune system. Immature T-cells arrive from your bone marrow - millions of them every day. The thymus puts them through rigorous training and quality control.
About 98% of these trainee cells fail. They're either too weak to recognize threats or too aggressive, likely to attack your own tissues. The thymus eliminates them. The 2% that pass get deployed throughout your body as part of your adaptive immune system.
These thymic graduates, called naive T-cells, can recognize pathogens your body has never encountered before. They're different from memory T-cells, which only recognize threats you've already fought off. As your thymus shrinks, your production of naive T-cells plummets. You're increasingly reliant on your existing immune memory - fine for old threats, but catastrophic for new ones.
This process, called thymic involution, begins surprisingly early. Your thymus is already shrinking by age one. It's most active during childhood and adolescence, when you're building your immune repertoire. After puberty, it starts replacing functional tissue with fat at about 3% per year.
By age 60, most people's thymuses are barely functional. They produce perhaps 1% of the naive T-cells they made at age 20. This decline tracks almost perfectly with increased vulnerability to infections, reduced vaccine effectiveness, and rising cancer rates.

Scientists are pursuing thymus regeneration through several distinct approaches, each targeting different aspects of thymic biology.
Hormonal therapies like the TRIIM protocol work by manipulating growth signals. Growth hormone stimulates thymic epithelial cells - the specialized cells that create the thymus's training environment. DHEA and other sex hormones also play a role, which helps explain why castration in animals delays thymic involution.
But hormones are a blunt instrument. They affect tissues throughout the body, not just the thymus. That's why TRIIM includes metformin, a diabetes drug that helps mitigate growth hormone's tendency to increase insulin resistance.
Protein therapies offer more precision. Researchers at Edinburgh University discovered that a protein called FOXN1 controls thymic development. When they injected recombinant FOXN1 into aged mice, thymic function improved measurably. The organ didn't just stop shrinking - it started producing more T-cells again.
Other protein candidates include BMP4 (bone morphogenetic protein 4), which promotes thymic regeneration after damage, and IL-22 (interleukin-22), which stimulates thymic epithelial cell growth.
Cell-based therapies take things further. Instead of stimulating existing thymic cells, scientists are building new ones from scratch. University College London researchers engineered functional thymus tissue from human stem cells in 2020. When transplanted into mice, the bioengineered tissue supported T-cell development just like a natural thymus.
This approach could eventually allow doctors to transplant lab-grown thymic tissue into patients whose thymuses have completely atrophied. The tissue could be made from the patient's own cells, eliminating rejection risk.
Stem cell approaches leverage the thymus's own repair mechanisms. Recent research identified thymic epithelial progenitor cells - specialized stem cells that can regenerate thymic tissue. Understanding how to activate these dormant progenitors could provide a way to trigger regeneration from within.
The path from promising research to available treatment is long, but several therapies are already in human trials.
Beyond TRIIM-X, pharmaceutical companies are testing small molecules that stimulate thymic regeneration. One compound, a RANKL agonist, restored thymic function and improved immune responses in aged mice. Human trials are planned for 2025.
Gene therapy approaches are also advancing. Scientists are exploring ways to deliver FOXN1 directly to thymic cells using viral vectors, potentially providing sustained regeneration without repeated treatments.
The timeline for clinical availability depends on which approach you're considering. The TRIIM protocol uses already-approved drugs in new combinations, which could accelerate regulatory approval if TRIIM-X succeeds. Some longevity clinics already offer similar protocols off-label, though this practice remains controversial.
Protein therapies and bioengineered tissue will likely take longer - perhaps 10-15 years before widespread availability. Regulatory agencies require extensive safety data for novel biological products, and manufacturing bioengineered organs at scale presents formidable technical challenges.
But the momentum is undeniable. Thymus regeneration was a niche research topic five years ago. Today, it's become a major focus in aging research, with substantial funding from longevity-focused organizations and pharmaceutical companies.
While much attention focuses on healthy aging, thymus regeneration could transform treatment for several conditions.
Cancer immunotherapy depends on robust T-cell responses. Patients undergoing chemotherapy often experience severe thymic damage, which permanently impairs their immune systems. Regenerating the thymus after cancer treatment could restore immune function and reduce infection risk during recovery.
Some cancer immunotherapies, like CAR-T cell therapy, require harvesting and engineering a patient's own T-cells. Elderly patients often don't have enough functional T-cells for these approaches to work. Thymic regeneration could expand eligibility for these life-saving treatments.
Autoimmune diseases result partly from defective thymic selection - the boot camp lets through T-cells that attack the body's own tissues. New research suggests that regenerating the thymus with proper function might help reset immune tolerance in some autoimmune conditions.
Vaccine effectiveness declines sharply with age because elderly immune systems can't generate robust responses to new antigens. This isn't just about COVID-19 or flu. It's shingles, pneumonia, and emerging infectious diseases. Thymic regeneration could restore vaccine responsiveness, potentially saving millions of lives.
One researcher noted that diminished thymic function likely explains why COVID-19 vaccines showed reduced efficacy in the oldest age groups. If we could regenerate the thymus before vaccination, even elderly individuals might mount youthful immune responses.
HIV and other infectious diseases that target the immune system could also benefit. HIV damages the thymus, progressively reducing T-cell production. Thymic regeneration could help patients maintain stronger immune systems even while managing chronic infection.

Not everything is optimistic. Thymus regeneration faces significant hurdles.
Safety concerns top the list. Growth hormone can increase cancer risk and insulin resistance. While TRIIM's metformin component helps manage these effects, long-term safety data is sparse. The trial only followed participants for one year. What happens after five years? Ten?
The thymus itself raises safety questions. Could regenerating it too aggressively lead to autoimmune problems? The thymus eliminates self-reactive T-cells, but this quality control isn't perfect. Flooding the body with newly trained T-cells might increase autoimmunity risk.
Individual variability complicates treatment. People's thymuses don't all decline at the same rate. Genetics, lifestyle, and environmental factors all play roles. Smoking, for instance, accelerates thymic involution, while exercise may slow it. Personalized dosing will be essential.
Cost and accessibility will determine who benefits. Bioengineered thymus tissue, if it becomes available, will likely cost hundreds of thousands of dollars initially. Even simpler hormone-based approaches could be expensive if not covered by insurance. This technology could exacerbate health disparities between wealthy and poor populations.
Regulatory pathways remain unclear. Should thymic regeneration be considered a treatment for aging, or does it need to target specific diseases? Most regulatory agencies don't recognize aging as a treatable condition, which complicates approval for interventions that primarily slow or reverse aging processes.
There's also the question of what "normal" means. If we can regenerate thymuses to youthful levels, should we aim for the thymic function of a 20-year-old, a 30-year-old, or something in between? Too much immune activity could increase inflammation and autoimmune risk.
Different regions approach thymus regeneration research with distinct priorities.
The United States leads in clinical trials and entrepreneurial longevity medicine. Private funding dominates, with billionaire-backed initiatives like the Hevolution Foundation investing hundreds of millions in aging research. This creates rapid innovation but also raises concerns about equitable access.
Europe takes a more regulated approach, with substantial public funding through the European Research Council. European researchers have pioneered much of the fundamental biology of thymic aging and are leaders in bioengineered organ development. The region's universal healthcare systems might enable broader access once treatments are approved.
Japan faces unique demographic pressures. With the world's oldest population, Japan has strong incentives to develop interventions that maintain health in the elderly. Japanese researchers contribute significantly to immunosenescence research, with particular focus on maintaining quality of life in advanced age.
China is investing heavily in stem cell research and regenerative medicine, with less restrictive regulatory environments for experimental therapies. This could accelerate development but raises ethical concerns about safety oversight.
Developing nations face different challenges. Where infectious disease remains a major killer, interventions that boost immune function could have enormous public health impact - but only if made affordable and accessible.
What can individuals do while waiting for thymus regeneration therapies to mature?
First, understand that lifestyle affects thymic health. Chronic stress accelerates thymic involution through elevated cortisol levels. Exercise appears protective - active older adults maintain better thymic function than sedentary peers. Nutrition matters too, with protein intake and certain micronutrients supporting thymic health.
Second, stay informed about clinical trials. ClinicalTrials.gov lists ongoing studies, and some may be accepting participants. Participating in research not only provides early access to potential therapies but contributes to scientific knowledge.
Third, advocate for research funding and regulatory frameworks that support longevity medicine. The pace of progress depends partly on public support for aging research and policies that facilitate clinical translation.
Finally, maintain perspective. Thymus regeneration won't create immortality or eliminate all age-related disease. It's one piece of a larger puzzle. But it's a crucial piece - one that could meaningfully extend healthy lifespan and reduce suffering from infectious disease, cancer, and immune decline.
The immune system touches virtually every aspect of health. A therapy that restores it to youthful function could ripple through medicine in ways we're only beginning to imagine. That's not hype. That's the logical consequence of fixing a system that's been broken since puberty.
We're approaching a fundamental shift in how we think about aging. For most of human history, immune decline was inevitable - something to accept and manage. Within the next decade, it might become optional. The question isn't whether we can regenerate the thymus. It's whether we'll make that option available to everyone who could benefit, not just those who can afford it.

Ahuna Mons on dwarf planet Ceres is the solar system's only confirmed cryovolcano in the asteroid belt - a mountain made of ice and salt that erupted relatively recently. The discovery reveals that small worlds can retain subsurface oceans and geological activity far longer than expected, expanding the range of potentially habitable environments in our solar system.

Scientists discovered 24-hour protein rhythms in cells without DNA, revealing an ancient timekeeping mechanism that predates gene-based clocks by billions of years and exists across all life.

3D-printed coral reefs are being engineered with precise surface textures, material chemistry, and geometric complexity to optimize coral larvae settlement. While early projects show promise - with some designs achieving 80x higher settlement rates - scalability, cost, and the overriding challenge of climate change remain critical obstacles.

The minimal group paradigm shows humans discriminate based on meaningless group labels - like coin flips or shirt colors - revealing that tribalism is hardwired into our brains. Understanding this automatic bias is the first step toward managing it.

In 1977, scientists discovered thriving ecosystems around underwater volcanic vents powered by chemistry, not sunlight. These alien worlds host bizarre creatures and heat-loving microbes, revolutionizing our understanding of where life can exist on Earth and beyond.

Automated systems in housing - mortgage lending, tenant screening, appraisals, and insurance - systematically discriminate against communities of color by using proxy variables like ZIP codes and credit scores that encode historical racism. While the Fair Housing Act outlawed explicit redlining decades ago, machine learning models trained on biased data reproduce the same patterns at scale. Solutions exist - algorithmic auditing, fairness-aware design, regulatory reform - but require prioritizing equ...

Cache coherence protocols like MESI and MOESI coordinate billions of operations per second to ensure data consistency across multi-core processors. Understanding these invisible hardware mechanisms helps developers write faster parallel code and avoid performance pitfalls.