Antibacterial Soap May Be Destroying Your Gut Health

TL;DR: Peroxisomes are cellular organelles that perform critical metabolic functions yet remain poorly understood. When they malfunction, they cause devastating diseases from severe infant conditions like Zellweger syndrome to adult disorders like adrenoleukodystrophy. New research is finally revealing their importance.

Inside each of your cells are microscopic powerhouses that nobody talks about. While mitochondria get called the "powerhouse of the cell" in every biology class and lysosomes are known as cellular recycling centers, another organelle performs over 50 critical biochemical reactions yet remains virtually invisible to the public. These are peroxisomes, and when they fail, the consequences devastate lives in ways that have puzzled physicians for decades.
Peroxisomes were first spotted in 1954 by Swedish doctoral student J. Rhodin, but weren't officially identified as distinct organelles until 1966 when Christian de Duve and Pierre Baudhuin gave them their name. These membrane-bound structures measure just 0.1 to 1 micrometer in diameter, yet they're essential for life.
Think of peroxisomes as your cell's specialized chemical factories. They break down very long chain fatty acids that mitochondria can't handle, synthesize plasmalogens that form the insulating myelin sheaths around your nerves, and neutralize the reactive oxygen species that would otherwise damage cellular components. The organelles perform beta-oxidation of fatty acids, generate bile acids necessary for digestion, and even play a role in your body's antiviral defenses.
What makes peroxisomes unique is their oxidative nature. They deliberately generate hydrogen peroxide during their metabolic reactions, then immediately break it down with catalase enzymes before it can harm the cell. It's like having a controlled fire that provides energy without burning down the house.
Peroxisomes perform over 50 different biochemical reactions inside your cells, yet remain virtually unknown outside specialized research labs.
Despite their discovery nearly 60 years ago, peroxisomes remain obscure even among healthcare professionals. There are several reasons for this scientific neglect.
First, the diseases caused by peroxisomal dysfunction are rare. Zellweger syndrome, the most severe peroxisomal disorder, affects roughly 1 in 50,000 births. Compare that to mitochondrial diseases that collectively affect about 1 in 4,300 people. Rare diseases attract less research funding and fewer headlines.
Second, peroxisomal disorders present with bewildering variety. The same organelle dysfunction can cause severe seizures in infants, progressive blindness in children, or adult-onset neurological decline. This clinical heterogeneity made it difficult for physicians to recognize these conditions as related, so they were often classified separately until genetic testing revealed their common origin.
Third, peroxisomes were discovered during a period when mitochondria were the hot topic in cell biology. Mitochondrial research dominated scientific attention and funding, leaving their smaller cousins in the shadows. Even today, a search for "mitochondrial disease" yields vastly more results than "peroxisomal disorder."
The complexity of peroxisomal biogenesis also posed research challenges. Building a functional peroxisome requires at least 36 different peroxin proteins encoded by PEX genes. Mutations in any of these genes can disrupt peroxisome formation, creating a genetic puzzle that took decades to unravel.
When peroxisomes malfunction, metabolic chaos ensues across multiple systems. The consequences cascade through the body in ways that seem unrelated until you understand the organelle's diverse roles.
The most immediate effect is the accumulation of very long chain fatty acids (VLCFAs) in the blood and tissues. These molecules, containing 22 or more carbon atoms, normally get shortened by peroxisomal beta-oxidation. Without functional peroxisomes, VLCFAs build up in cell membranes, particularly in the brain and adrenal glands. This disrupts membrane structure, interferes with cell signaling, and triggers inflammation.
The brain suffers especially because it depends on plasmalogens, specialized phospholipids that make up nearly 20% of myelin. Peroxisomes synthesize plasmalogens, so their dysfunction causes defective myelination. The protective sheaths around nerves don't form properly, leading to seizures, developmental delays, and progressive neurological decline. Research shows that plasmalogen deficiency contributes to dementia and Alzheimer's disease, suggesting peroxisomal health may influence common neurodegenerative conditions.
"Normal plasma VLCFA levels were observed in a patient with a peroxisome biogenesis disorder, challenging the assumption that VLCFA elevation is universal in these conditions."
- BMC Pediatrics, 2024
Peroxisomes also produce bile acids essential for fat digestion and vitamin absorption. When this pathway fails, patients develop liver dysfunction and struggle to absorb fat-soluble vitamins A, D, E, and K. Vision problems emerge from vitamin A deficiency, bones weaken from vitamin D deficiency, and bleeding disorders develop from vitamin K deficiency.

The organelles' role in neutralizing reactive oxygen species means their failure allows oxidative stress to damage cellular components. Proteins become dysfunctional, lipids oxidize, and DNA accumulates mutations. This accelerates aging processes and increases cancer risk.
Interestingly, the biochemical markers used for diagnosis can vary with age. A recent case report described a 10-year-old patient with confirmed peroxisome biogenesis disorder whose plasma VLCFA levels were completely normal, something that shouldn't happen according to textbooks. This finding suggests current diagnostic approaches miss cases, especially in older patients.
Peroxisomal disorders exist on a spectrum from devastating to manageable, depending on the degree of organelle dysfunction.
At the severe end lies Zellweger syndrome, where peroxisomes are essentially absent. Affected infants are born with distinctive facial features, profound hypotonia (floppiness), seizures that don't respond to medication, and liver disease. They typically die within the first year. Brain imaging reveals abnormal migration of neurons during development, and autopsy studies show virtually no myelin formation.
Within the Zellweger spectrum disorders, milder variants allow survival into childhood or adolescence. These children experience developmental delays, hearing loss, retinal degeneration leading to blindness, and gradual neurological deterioration. Some develop autism spectrum features, though the connection between peroxisomal dysfunction and autism remains an active research area.
Adrenoleukodystrophy (ALD), popularized by the 1992 film "Lorenzo's Oil," results from mutations in a single peroxisomal protein rather than complete organelle failure. The X-linked form affects boys who develop normally until age 4-10, then experience rapid neurological decline as myelin throughout the brain disintegrates. Adult men with the same mutation may develop a slowly progressive form called adrenomyeloneuropathy that affects the spinal cord and causes progressive weakness and spasticity.
The same genetic mutations can cause severe infant death or mild adult symptoms, depending on how much residual peroxisome function remains.
Refsum disease represents the mildest end of the spectrum. Patients accumulate phytanic acid from dietary sources because peroxisomes can't break it down. Symptoms typically begin in adolescence or early adulthood with night blindness, loss of smell, hearing loss, and peripheral neuropathy. Unlike Zellweger syndrome, Refsum disease is treatable through dietary restriction of phytanic acid and plasmapheresis to remove accumulated molecules from the blood.

The variability within peroxisomal disorders depends on residual organelle function. Complete absence causes early death, while partial function allows longer survival with chronic symptoms. Mutations in different PEX genes produce different phenotypes, though the exact genotype-phenotype correlations remain incompletely understood.
Peroxisomal disorders are notoriously difficult to diagnose, and many cases go unrecognized until genetic testing reveals the truth.
The clinical presentations overlap with dozens of other conditions. An infant with seizures and developmental delay might be evaluated for epilepsy, cerebral palsy, or mitochondrial disease before anyone considers peroxisomes. The facial features seen in Zellweger syndrome are subtle and can be missed without expertise in dysmorphology.
Biochemical testing for elevated VLCFAs is the traditional first-line diagnostic approach, but it has limitations. As the recent case report demonstrated, plasma VLCFA levels can be normal even in confirmed peroxisomal disorders, particularly in older patients. Plasmalogen levels are more sensitive but harder to measure and not widely available.
Genetic testing has revolutionized diagnosis but introduces new challenges. There are at least 36 PEX genes plus genes for individual peroxisomal enzymes, creating enormous genetic heterogeneity. Whole-exome sequencing increasingly identifies variants of uncertain significance, leaving families in diagnostic limbo while researchers work to classify their pathogenicity.
Newborn screening programs don't routinely test for peroxisomal disorders in most countries. The rarity of these conditions and the costs of screening have kept them off most panels, though pilot programs are exploring their inclusion. Early diagnosis would enable supportive care and genetic counseling before irreversible damage occurs.
Neuroimaging provides valuable clues. MRI often shows characteristic patterns of abnormal white matter, impaired myelination, and brain malformations. However, these findings aren't specific enough for diagnosis without biochemical or genetic confirmation.
The diagnostic odyssey for families can last years. Parents watch their child struggle while moving from specialist to specialist, accumulating inconclusive test results. The psychological toll is enormous, and delayed diagnosis means missed opportunities for intervention and family planning.
There's no cure for peroxisomal disorders, but treatment strategies aim to slow progression and manage symptoms.
For adrenoleukodystrophy, the treatment landscape has evolved dramatically. Lorenzo's oil, a 4:1 mixture of oleic acid and erucic acid, was developed by Augusto and Michaela Odone for their son Lorenzo in the 1980s. While it reduces plasma VLCFA levels, its clinical benefits remain controversial. Studies suggest it may delay symptom onset when started presymptomatically but doesn't stop progression once neurological symptoms begin.
Hematopoietic stem cell transplantation has become the standard treatment for boys with ALD who have early brain involvement. The procedure replaces the patient's immune system with donor cells that can produce the missing protein and halt inflammatory demyelination. Success depends on catching the disease early, before extensive brain damage occurs. The transplant itself carries significant risks, including death, but can preserve neurological function in carefully selected patients.
"Lorenzo's oil contributed to treatment of a devastating disease, but its clinical efficacy remains debated decades after its development."
- McGill Office for Science and Society
For Refsum disease, dietary management works remarkably well. Patients avoid foods high in phytanic acid, particularly dairy products, ruminant meats, and certain fish. Combined with occasional plasmapheresis to remove accumulated phytanic acid, this approach can prevent or even reverse some symptoms like peripheral neuropathy.
Supportive care forms the backbone of treatment for most peroxisomal disorders. This includes physical therapy to maintain function, antiepileptic drugs for seizures, hearing aids, vitamin supplementation, and treatment of liver dysfunction. Specialized metabolic centers coordinate multidisciplinary care and connect families with resources.
Experimental treatments offer hope. Gene therapy approaches aim to deliver functional copies of mutated genes using viral vectors. Early-phase clinical trials are underway for some peroxisomal disorders, building on successes in other genetic diseases. CRISPR-based gene editing might eventually allow correction of mutations directly in patients' cells.
Substrate reduction therapy attempts to decrease the production of molecules that accumulate when peroxisomes fail. If you can't break down VLCFAs efficiently, perhaps you can reduce their synthesis. Small molecule drugs targeting fatty acid elongation enzymes are being developed based on this principle.
Peroxisome biogenesis enhancement represents another strategy. Could we boost the function of partially working peroxisomes? Research into small molecules that increase PEX gene expression or improve peroxisomal protein import shows promise in laboratory models.
Scientific interest in peroxisomes is experiencing a renaissance as researchers recognize their broader relevance to human health.
New connections are emerging between peroxisomal dysfunction and common diseases. Recent studies link plasmalogen deficiency to Alzheimer's disease, suggesting peroxisomal health influences neurodegenerative disease risk even in people without genetic peroxisomal disorders. Could optimizing peroxisome function protect against dementia?
The organelles' role in innate immunity is attracting attention. Peroxisomes serve as platforms for antiviral signaling, and some viruses specifically target them to evade immune responses. Understanding this interaction might reveal new antiviral strategies.
Peroxisome dysfunction may contribute to aging. The organelles' ability to neutralize reactive oxygen species declines with age, potentially contributing to age-related diseases. Research into compounds that boost peroxisomal function shows promise for healthy aging interventions.
Emerging research suggests peroxisomal health may influence common conditions like Alzheimer's disease, expanding their relevance beyond rare genetic disorders.
Advanced imaging techniques are revealing peroxisomal dynamics in living cells. Super-resolution microscopy shows how these organelles move, divide, and interact with other cellular structures in real-time. This is unveiling their roles in processes we didn't previously associate with peroxisomes.
Patient advocacy organizations like The Global Foundation for Peroxisomal Disorders are raising awareness and funding research. These groups connect families, provide resources, and push for newborn screening inclusion. Their efforts are slowly bringing peroxisomal disorders out of obscurity.
The development of cellular models and model organisms accelerates research. Patient-derived induced pluripotent stem cells can be differentiated into neurons or other affected cell types, allowing researchers to study disease mechanisms and test potential therapies. Zebrafish and fruit fly models with peroxisomal defects provide systems for drug screening.
The story of peroxisomes illustrates how scientific attention shapes medical progress. These organelles were discovered at the same time as many others but received a fraction of the research investment. The consequence has been decades of diagnostic delays, limited treatment options, and families struggling without answers.
As genomic sequencing becomes routine, we're identifying peroxisomal disorders more frequently. Cases that would have remained mysterious are now getting diagnosed, revealing that these conditions may be more common than previously thought. This rising case count is driving renewed research interest.
The biochemical pathways involving peroxisomes intersect with those of mitochondria, endoplasmic reticulum, and lysosomes. Understanding peroxisomal disorders is teaching us about organellar cooperation and how cellular metabolism is orchestrated. This knowledge applies beyond rare diseases to common conditions involving metabolic dysfunction.
For patients and families affected by peroxisomal disorders, the landscape is slowly improving. Diagnostic methods are getting better, treatment options are expanding, and research is accelerating. While we're not yet at the point of cures, we're moving from hopelessness to realistic optimism.
The broader lesson is about scientific attention and funding priorities. Rare diseases affecting small numbers receive little research investment compared to common conditions, yet they often illuminate fundamental biology. The COVID-19 pandemic demonstrated how quickly science can move when resources are mobilized. Imagine what could be achieved if even a fraction of that attention turned to the hundreds of rare diseases still waiting for their moment in the spotlight.
Peroxisomes are finally emerging from obscurity. These tiny organelles, forgotten by science for too long, are revealing themselves as key players in health and disease. For the families who have been living with the consequences of peroxisomal dysfunction, this rediscovery can't come soon enough.
Rotating detonation engines use continuous supersonic explosions to achieve 25% better fuel efficiency than conventional rockets. NASA, the Air Force, and private companies are now testing this breakthrough technology in flight, promising to dramatically reduce space launch costs and enable more ambitious missions.

Triclosan, found in many antibacterial products, is reactivated by gut bacteria and triggers inflammation, contributes to antibiotic resistance, and disrupts hormonal systems - but plain soap and water work just as effectively without the harm.

AI-powered cameras and LED systems are revolutionizing sea turtle conservation by enabling fishing nets to detect and release endangered species in real-time, achieving up to 90% bycatch reduction while maintaining profitable shrimp operations through technology that balances environmental protection with economic viability.

The pratfall effect shows that highly competent people become more likable after making small mistakes, but only if they've already proven their capability. Understanding when vulnerability helps versus hurts can transform how we connect with others.

Leafcutter ants have practiced sustainable agriculture for 50 million years, cultivating fungus crops through specialized worker castes, sophisticated waste management, and mutualistic relationships that offer lessons for human farming systems facing climate challenges.

Gig economy platforms systematically manipulate wage calculations through algorithmic time rounding, silently transferring billions from workers to corporations. While outdated labor laws permit this, European regulations and worker-led audits offer hope for transparency and fair compensation.
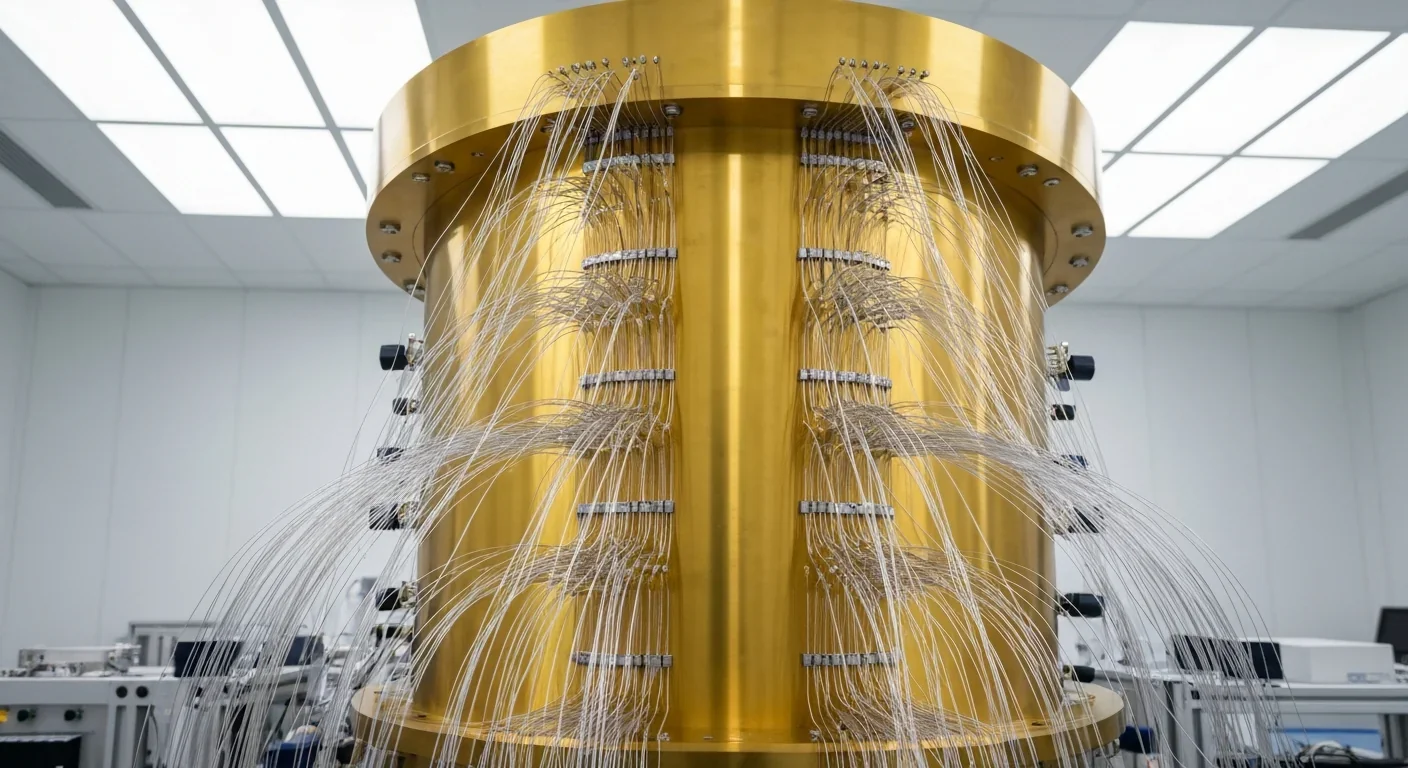
Quantum computers face a critical but overlooked challenge: classical control electronics must operate at 4 Kelvin to manage qubits effectively. This requirement creates engineering problems as complex as the quantum processors themselves, driving innovations in cryogenic semiconductor technology.