The Ancient Protein Clock That Ticks Without DNA

TL;DR: Scientists are discovering that a microscopic sugar coating called the glycocalyx lines our blood vessels and acts as the first defense against heart disease. When damaged by diabetes, inflammation, or aging, this protective layer breaks down and triggers atherosclerosis, but emerging therapies show it can be restored.

In a quiet revolution happening inside your blood vessels right now, scientists are uncovering why traditional risk factors like cholesterol and blood pressure tell only half the story. The real action is taking place at a molecular level so small it was invisible to researchers until recently: a sugar-based coating called the glycocalyx that lines every blood vessel in your body. When this protective layer breaks down, it doesn't just signal trouble, it actively triggers the cascade of events that leads to heart attacks and strokes.
Think of the glycocalyx as bubble wrap for your blood vessels. This gel-like layer, typically 0.5 to 4.5 micrometers thick, coats the inside of every artery and vein in your circulatory system. It's composed of an intricate network of proteoglycans and glycoproteins, complex molecules that stick out from the endothelial cells like tiny trees in a molecular forest.
The structure consists of core proteins with attached sugar chains called glycosaminoglycans, primarily heparan sulfate and chondroitin sulfate. These negatively charged sugar molecules create an electrostatic barrier that repels blood cells and platelets, preventing them from sticking to vessel walls.
But the glycocalyx does far more than just provide a physical barrier. It acts as a mechanosensor, detecting changes in blood flow and triggering the release of nitric oxide, the molecule that keeps blood vessels relaxed and open. It regulates inflammation by controlling which white blood cells can access the vessel wall. It manages fluid balance by preventing plasma from leaking into tissues. And it protects against oxidative stress by neutralizing harmful free radicals before they can damage endothelial cells.
When researchers at Stanford University studied brain aging, they discovered that glycocalyx breakdown doesn't just happen in diseased vessels, it's a key driver of the aging process itself. The thinner your glycocalyx, the faster your blood vessels age.
The glycocalyx exists in a constant state of renewal and repair, with components being shed and rebuilt continuously. But certain conditions accelerate degradation faster than the body can rebuild it.
Hyperglycemia, the elevated blood sugar seen in diabetes, triggers multiple destructive pathways simultaneously. High glucose levels activate enzymes called matrix metalloproteinases that literally chew through glycocalyx proteins. Sugar molecules bind to glycocalyx components through a process called glycation, making them stiff and dysfunctional. Research shows that even short-term spikes in blood sugar can cause measurable glycocalyx thinning within hours.
Chronic inflammation releases an enzyme called heparanase that specifically targets heparan sulfate, the most abundant component of the glycocalyx. During severe infections or sepsis, heparanase activity can strip the glycocalyx down to nothing in a matter of hours. The enzyme acts like molecular scissors, snipping the long sugar chains into fragments that drift away in the bloodstream.
Oxidative stress from smoking, pollution, or metabolic dysfunction generates reactive oxygen species that attack the delicate sulfate groups on glycocalyx sugars. Once damaged, these molecules lose their negative charge and can no longer repel blood cells. The protective barrier collapses.
Hypertension creates shear stress that physically tears glycocalyx components from the vessel wall. Think of it like wind eroding a cliff face. The faster the blood flows and the higher the pressure, the more rapid the erosion. Studies measuring syndecan-1, a key glycocalyx protein, found levels 25 times higher in patients with severe vascular disease compared to healthy controls, evidence of massive shedding.
But here's what makes glycocalyx degradation so insidious: these processes feed on each other. Inflammation triggers oxidative stress. Oxidative stress damages the glycocalyx, which allows more inflammatory cells to access the vessel wall, which creates more inflammation. It's a vicious cycle that accelerates over time.
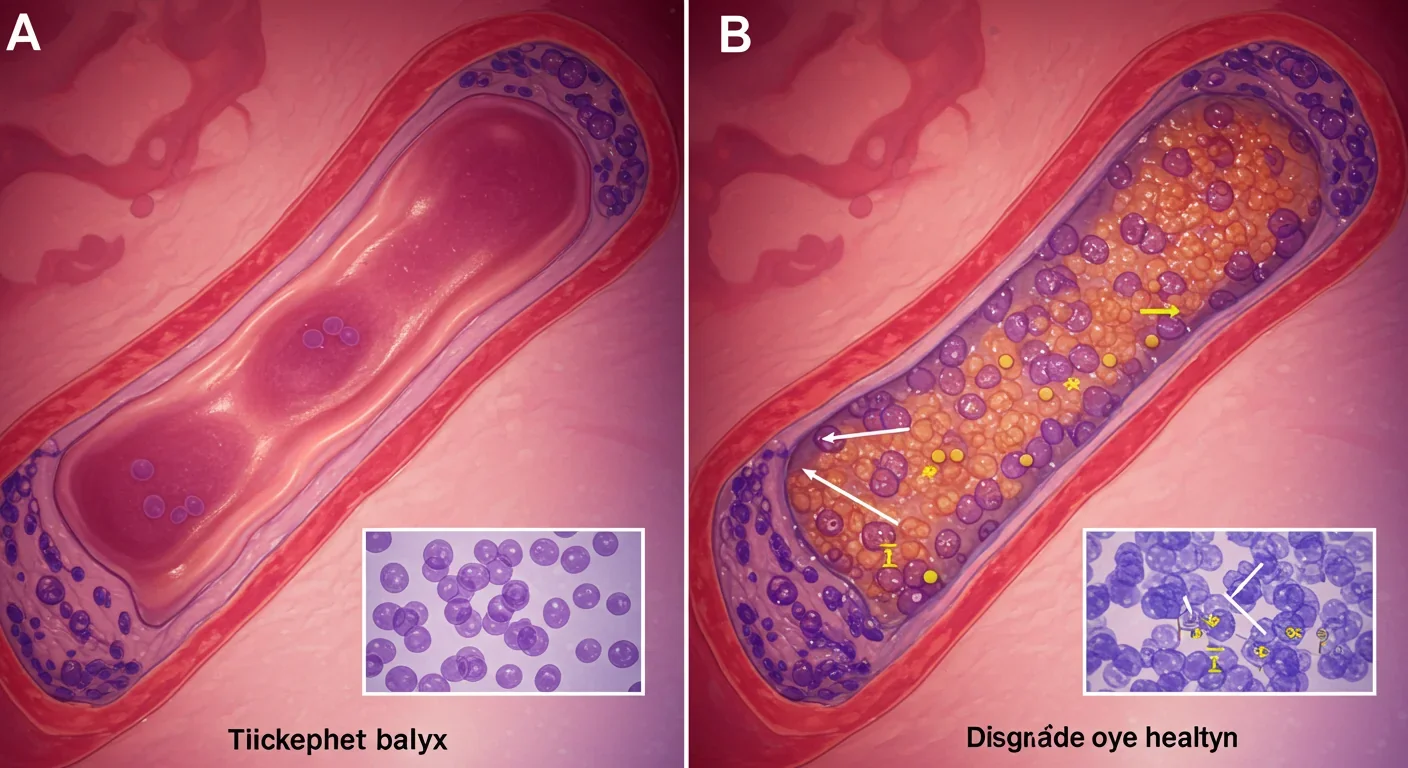
When the glycocalyx thins or disappears, the consequences ripple through every aspect of vascular function.
Loss of the barrier function allows albumin and other plasma proteins to leak into the vessel wall, causing edema and swelling. White blood cells that would normally slide past now stick and burrow into the endothelium, carrying inflammatory chemicals deep into the arterial wall. Platelets begin adhering to exposed endothelial surfaces, forming the seeds of blood clots.
Mechanosensing fails, which means endothelial cells can no longer detect blood flow properly. Nitric oxide production drops, causing vessels to constrict rather than dilate in response to increased demand. Theoretical models show that even a 50% reduction in glycocalyx thickness can cut nitric oxide bioavailability by more than 70%. This explains why patients with glycocalyx damage develop hypertension even when other risk factors are controlled.
Inflammatory signaling spirals out of control. Normally, the glycocalyx sequesters inflammatory molecules, keeping them away from endothelial receptors. Without this buffer, every inflammatory signal gets amplified. The vessel wall becomes a war zone of immune activity, with macrophages accumulating and releasing enzymes that further degrade the extracellular matrix.
Coagulation shifts toward clotting. The glycocalyx normally presents anticoagulant molecules like antithrombin and tissue factor pathway inhibitor on its surface. When these disappear, the balance tips toward thrombosis. Research on sepsis patients shows that glycocalyx loss precedes and predicts the development of disseminated intravascular coagulation, a catastrophic clotting disorder.
All of these changes create the perfect conditions for atherosclerosis. LDL cholesterol, which would normally be repelled by the glycocalyx's negative charge, now penetrates freely into the arterial wall where it becomes oxidized and engulfed by macrophages. The foam cells that result are the hallmark of early atherosclerotic plaques.
For years, the glycocalyx remained more theoretical than practical because we couldn't measure it in living patients. That's changing.
Biomarker tests detect shed glycocalyx components in blood. Syndecan-1 levels measured by ELISA correlate with disease severity across multiple conditions, from heart failure to COVID-19. Elevated levels indicate active glycocalyx degradation happening somewhere in the body. Hyaluronic acid fragments and heparan sulfate breakdown products serve similar functions.
Advanced imaging techniques can now visualize the glycocalyx directly. Sidestream dark-field imaging uses reflected light to measure glycocalyx thickness in sublingual blood vessels, a proxy for systemic health. Perfused boundary region analysis quantifies the permeable zone where red blood cells can penetrate the glycocalyx. Studies using these methods show measurable differences between healthy people and those with diabetes or hypertension.
Functional tests assess how well the glycocalyx is doing its job. Measuring how quickly albumin leaks from capillaries after a standardized stress gives insight into barrier function. Tracking how nitric oxide production responds to changes in blood flow reveals mechanosensing capacity.
These tools are moving from research labs into clinical practice. Within the next few years, your doctor might check your glycocalyx health as routinely as checking cholesterol, providing an early warning system for vascular disease before irreversible damage occurs.
The good news? The glycocalyx is dynamic. Damage it, and the body immediately starts rebuilding. Support that repair process, and you can restore function even after significant degradation.
Dietary interventions provide the raw materials for glycocalyx synthesis. The precursor molecules are simple: glucosamine, N-acetylglucosamine, and glucuronic acid. A 2024 clinical trial found that supplementing these glycocalyx building blocks improved vascular function in type 2 diabetics within eight weeks. Blood flow increased, inflammation markers dropped, and endothelial function normalized.
Antioxidants protect existing glycocalyx from oxidative damage. Not the megadose supplements that studies keep debunking, but the natural compounds found in colorful vegetables: anthocyanins from berries, polyphenols from green tea, sulforaphane from broccoli. These molecules neutralize reactive oxygen species before they can attack sulfate groups.
Exercise emerges as one of the most potent glycocalyx therapies. The shear stress from increased blood flow during activity triggers endothelial cells to produce more glycocalyx components. Regular aerobic exercise actually thickens the glycocalyx over time. Research shows that athletes have glycocalyx measurements 30-40% better than sedentary controls of the same age.
Pharmaceutical approaches target specific degradation pathways. Sulodexide, a mixture of glycosaminoglycans extracted from porcine intestine, provides material for glycocalyx repair. Animal studies demonstrate that sulodexide treatment reduces glycocalyx shedding, improves barrier function, and protects against organ damage in sepsis models. It activates cellular signaling pathways that enhance both synthesis and reduce breakdown.
Heparanase inhibitors block the enzyme that degrades heparan sulfate. Multiple compounds are in clinical trials for cancer, where heparanase helps tumors spread, but their cardiovascular benefits are becoming apparent. By preventing enzymatic destruction, these drugs allow the body's natural repair mechanisms to get ahead.
Glycemic control remains fundamental. Every point reduction in hemoglobin A1c correlates with measurable glycocalyx improvement. Medications like GLP-1 agonists that improve blood sugar while reducing inflammation show particularly strong glycocalyx benefits beyond their glucose effects.
One of the most striking recent discoveries links glycocalyx health to cognitive decline and dementia.
The blood-brain barrier is fundamentally a specialized glycocalyx structure. Brain capillaries have an exceptionally thick and complex glycocalyx layer that works with tight junctions between endothelial cells to keep the brain's environment pristine. Stanford researchers found that glycocalyx breakdown precedes blood-brain barrier failure in aging and Alzheimer's disease.
As the brain's glycocalyx thins, it allows plasma proteins to leak into neural tissue, triggering inflammation. Immune cells that should never enter the brain parenchyma slip through the compromised barrier. Amyloid beta, the protein that accumulates in Alzheimer's, normally gets cleared from the brain via transport proteins on the glycocalyx. When those disappear, clearance fails and plaques form.
This suggests that protecting your vascular glycocalyx doesn't just prevent heart attacks and strokes, it might preserve cognitive function as you age. The same interventions that improve cardiovascular health could be neuroprotective.
The COVID-19 pandemic revealed another critical role for the glycocalyx: defending against viral entry.
Many viruses, including SARS-CoV-2, use glycocalyx components as initial binding sites. Heparan sulfate on the endothelial surface helps concentrate viral particles near ACE2 receptors, facilitating infection. But here's the paradox: a healthy glycocalyx actually protects against severe disease by limiting how deep the virus penetrates and by maintaining barrier function that prevents systemic spread.
The patients who developed severe COVID-19 often had pre-existing glycocalyx damage from diabetes, hypertension, or obesity. Their compromised endothelial coating couldn't contain the infection, leading to widespread vascular inflammation and the blood clotting disorders that made COVID so deadly.

Herpes zoster reactivation triggers similar glycocalyx-mediated vascular damage, which may explain the increased risk of heart attacks and strokes in the months following shingles. The virus directly infects endothelial cells, inducing heparanase release that strips away the protective coating.
This connects to a broader principle: anything that damages the glycocalyx increases vulnerability to vascular complications from infections. Protecting your glycocalyx might be as important as vaccines for maintaining cardiovascular health during infectious disease exposure.
Perhaps nowhere is glycocalyx degradation more dramatic or consequential than in sepsis, the life-threatening response to infection.
Sepsis patients experience catastrophic glycocalyx shedding within hours of disease onset. Syndecan-1 levels can increase 50-fold as the protective coating is enzymatically destroyed. This shedding drives three major sepsis complications simultaneously.
Capillary leak occurs as barrier function collapses, allowing fluid to pour from blood vessels into tissues. Patients develop massive edema, their lungs fill with fluid, and blood pressure crashes despite aggressive fluid resuscitation. The leaked fluid doesn't stay in vessels because there's no glycocalyx to hold it.
Coagulopathy develops as the anticoagulant surface is lost and pro-thrombotic signals dominate. Microthrombi form throughout the body, consuming clotting factors and platelets, which paradoxically increases bleeding risk. It's a clotting and bleeding disorder at the same time.
Vasoplegia, the profound drop in vascular tone that makes septic shock so deadly, results from loss of glycocalyx-mediated mechanosensing. Blood vessels can't respond normally to pressure signals, leading to treatment-resistant hypotension.
Clinical trials testing glycocalyx-protective therapies in sepsis are showing promise. Treatments that reduce shedding or provide substrate for repair improve outcomes by addressing the fundamental vascular pathology rather than just treating symptoms.
The glycocalyx field is exploding with innovations that could transform cardiovascular medicine.
Glycocalyx-targeted imaging could replace invasive angiography for some applications. Contrast agents that specifically bind to damaged glycocalyx would light up vulnerable plaques before they rupture, identifying patients at immediate risk who appear stable by conventional measures.
Personalized glycocalyx profiling might reveal why some people develop heart disease despite perfect cholesterol and blood pressure while others remain healthy despite terrible risk factors. Genetic variations in glycocalyx synthesis or degradation enzymes could explain this variability.
Regenerative therapies are being developed that could rebuild degraded glycocalyx more completely than current approaches. Engineered glycocalyx mimetics, stem cell therapies that enhance endothelial repair capacity, and gene therapies that boost protective molecule production all show promise in early research.
Environmental medicine is starting to recognize glycocalyx damage as a mechanism linking pollution to cardiovascular disease. Particulate matter from traffic and industry generates oxidative stress that strips the glycocalyx. This suggests that air quality improvements could have cardiovascular benefits beyond what we currently measure.
Understanding glycocalyx biology forces us to rethink heart disease prevention.
Traditional approaches focus on reducing bad things: lowering cholesterol, decreasing blood pressure, losing weight. The glycocalyx perspective adds a new dimension: actively supporting vascular health by providing what the endothelium needs to maintain its protective coating.
It explains why lifestyle factors matter so much. Every meal, every workout, every night's sleep affects glycocalyx turnover. The cumulative effect of years of choices shows up in the thickness and quality of that sugar coating, which ultimately determines whether atherosclerosis develops or not.
It reveals why inflammation is central to cardiovascular disease, not just a consequence of it. Inflammatory enzymes actively destroy the barrier that normally prevents inflammatory cells from accessing vessel walls. Break down that barrier and you create a self-perpetuating cycle.
It offers hope for reversibility. Unlike arterial calcification or advanced fibrosis, a degraded glycocalyx can rebuild. Intervene early enough, support the repair process adequately, and you might not just slow disease progression but actually restore normal vascular function.
The hidden sugar coating that medical science barely acknowledged 20 years ago is becoming recognized as the first line of defense against the diseases that kill more people than any other. Protect your glycocalyx, and you might just protect your life.
What you eat for dinner tonight, whether you take that walk, how well you manage your blood sugar, these decisions don't just affect abstract lab values. They determine whether your body can maintain the molecular shield that keeps your vessels healthy. The glycocalyx is where prevention happens, at the interface between blood and vessel wall, in a layer so thin you need a microscope to see it but so important that your cardiovascular future depends on it.
Now that science has unveiled this hidden player, the question isn't whether to pay attention to glycocalyx health. It's how quickly we can translate that knowledge into interventions that prevent heart attacks and strokes before they happen. The tools are emerging. The understanding is solidifying. The opportunity is now.

Ahuna Mons on dwarf planet Ceres is the solar system's only confirmed cryovolcano in the asteroid belt - a mountain made of ice and salt that erupted relatively recently. The discovery reveals that small worlds can retain subsurface oceans and geological activity far longer than expected, expanding the range of potentially habitable environments in our solar system.

Scientists discovered 24-hour protein rhythms in cells without DNA, revealing an ancient timekeeping mechanism that predates gene-based clocks by billions of years and exists across all life.

3D-printed coral reefs are being engineered with precise surface textures, material chemistry, and geometric complexity to optimize coral larvae settlement. While early projects show promise - with some designs achieving 80x higher settlement rates - scalability, cost, and the overriding challenge of climate change remain critical obstacles.

The minimal group paradigm shows humans discriminate based on meaningless group labels - like coin flips or shirt colors - revealing that tribalism is hardwired into our brains. Understanding this automatic bias is the first step toward managing it.

In 1977, scientists discovered thriving ecosystems around underwater volcanic vents powered by chemistry, not sunlight. These alien worlds host bizarre creatures and heat-loving microbes, revolutionizing our understanding of where life can exist on Earth and beyond.

Automated systems in housing - mortgage lending, tenant screening, appraisals, and insurance - systematically discriminate against communities of color by using proxy variables like ZIP codes and credit scores that encode historical racism. While the Fair Housing Act outlawed explicit redlining decades ago, machine learning models trained on biased data reproduce the same patterns at scale. Solutions exist - algorithmic auditing, fairness-aware design, regulatory reform - but require prioritizing equ...

Cache coherence protocols like MESI and MOESI coordinate billions of operations per second to ensure data consistency across multi-core processors. Understanding these invisible hardware mechanisms helps developers write faster parallel code and avoid performance pitfalls.