Antibacterial Soap May Be Destroying Your Gut Health

TL;DR: Fecal microbiota transplantation (FMT) has evolved from experimental therapy to FDA-approved medicine, achieving 85-94% cure rates for recurrent C. difficile infections where antibiotics fail. The treatment transplants healthy gut bacteria from screened donors via colonoscopy, capsules, or enema, restoring microbial balance through competitive exclusion.

Within the next five years, more patients will receive fecal transplants from stool banks than from traditional donors, fundamentally transforming how we treat gut infections and potentially dozens of other conditions. What started as an experimental last resort for desperate patients has evolved into FDA-approved medicine with cure rates that make antibiotics look obsolete.
In 2013, researchers stopped a clinical trial early because continuing felt unethical. Patients receiving fecal microbiota transplantation (FMT) for recurrent Clostridium difficile infections showed an 81-94% cure rate, while those getting standard antibiotics managed only 31%. The difference was so dramatic that denying patients FMT seemed wrong.
This wasn't just another incremental improvement in medicine. FMT represents a completely different approach: instead of killing bacteria with antibiotics, you restore balance by transplanting an entire ecosystem of healthy microbes from donor stool into a sick person's gut.
The procedure works through what scientists call "competitive exclusion." When C. difficile bacteria colonize a gut depleted by antibiotics, they produce toxins that cause severe diarrhea, cramping, and potentially fatal inflammation. A healthy person's gut contains hundreds of bacterial species that normally keep C. diff in check. FMT delivers this protective community in a single treatment.
The concept isn't new. Chinese physicians in the 4th century administered "yellow soup" to treat severe diarrhea and food poisoning. But modern medicine dismissed fecal therapy for decades because of what researchers call the "ick factor."
That changed in 2013 when the FDA began regulating human feces as an experimental drug. This regulatory shift forced standardization of donor screening protocols and preparation methods, transforming FMT from a desperate experiment into legitimate medicine.
By November 2022, the FDA approved Rebyota, the first commercial FMT product, as a rectal suspension for preventing recurrent C. difficile infection. Four months later, Vowst became the first oral live biotherapeutic product approved for the same condition.
These approvals mark medicine's acceptance that sometimes the best cure involves donated poop.

Not everyone can donate stool for medical use. Donor screening starts with comprehensive questionnaires about medical history, medications, travel, sexual behavior, and recent illnesses. This eliminates most candidates immediately.
Those who pass face extensive laboratory testing. Blood tests screen for HIV, hepatitis B and C, syphilis, and other infectious diseases. Stool samples undergo analysis for parasites, pathogenic bacteria including Salmonella, Shigella, Campylobacter, and C. difficile itself. Labs also test for antibiotic-resistant organisms like MRSA and vancomycin-resistant Enterococcus.
Advanced screening includes metagenomic analysis to identify the donor's complete microbial profile. The best donors show high microbial diversity, typically including 57% Firmicutes, 24% Bacteroidota, and 18% Actinobacteriota, based on recent trials.
One study of 15 long-term donors found that higher donor diversity correlated directly with better clinical outcomes. Donors in the highest-quality tier achieved success rates exceeding 90%, while lower-diversity donors showed more variable results.
Fresh stool collection happens in specialized rooms using sterile containers that minimize air exposure. Within hours, technicians prepare the sample into a standardized suspension: 100 grams of stool diluted to 300 milliliters with phosphate-buffered saline, filtered through gauze to remove solid particles, then mixed with sterile glycerol at 25% concentration. The suspension gets frozen at -80°C for long-term storage.
Research shows frozen FMT performs equivalently to fresh material for treating recurrent C. difficile infection, making stool banking practical.
Three main delivery methods exist, each with distinct advantages.
Colonoscopy remains the traditional approach. During the procedure, physicians infuse 200-500 milliliters of thawed fecal suspension directly into the colon. This ensures the material reaches the lower intestine where C. diff primarily lives. Success rates exceed 90% with colonoscopic delivery, though the procedure requires bowel preparation, sedation, and carries small risks of perforation or bleeding.
Capsules offer a non-invasive alternative that patients strongly prefer. Freeze-dried microbes get packed into acid-resistant capsules that survive stomach acid and release in the intestines. Clinical trials show capsule FMT achieves 86% cure rates at one month, matching colonoscopy effectiveness without requiring sedation or hospital visits.
A 2022 study of 269 patients found no difference in cure rates between capsule and colonoscopic FMT. Dr. Byron Vaughn noted that "capsule FMT can avoid complications of colonoscopy and facilitate access to this potentially life-saving therapy."
Enema administration provides another option. Patients receive fecal suspension through rectal infusion, which they must retain for at least 30 minutes. A recent randomized trial showed rectal enema FMT achieved 73% clinical response for irritable bowel syndrome, slightly lower than capsules but still significantly better than placebo.
The thawed suspension must be administered within 6 hours to ensure microbial viability.

OpenBiome, founded in 2012, became America's first public stool bank and now supplies screened donor material to hundreds of hospitals. The stool bank model solves a critical problem: finding qualified donors is difficult, and screening costs hundreds of dollars per donor.
Centralized banks can screen donors once, then distribute their material widely, dramatically reducing costs and improving access. They maintain databases tracking donor microbiome profiles and clinical outcomes, enabling better donor-recipient matching.
However, FDA policy changes in 2022 created new challenges. The agency now exercises enforcement discretion only for stool prepared in healthcare facilities, not stool banks. This regulatory shift has made acquiring donor material more complex, pushing more physicians toward FDA-approved commercial products.
The FMTdb database now contains microbiome data from 370 FMT recipients, 15 long-term donors, and 2,008 healthy controls, available at http://gift2disease.net/FMTdb. This open-access resource helps researchers identify which donor profiles work best for specific conditions.
FMT's safety record looks remarkably good overall. A systematic review found serious adverse events occur in less than 1% of patients. Most side effects are mild: bloating, abdominal discomfort, nausea, and temporary diarrhea.
But "remarkably good" isn't the same as perfectly safe.
In 2019, two immunocompromised patients developed extended-spectrum beta-lactamase E. coli infections after receiving stool from the same donor. One patient died. The donor was an asymptomatic carrier of antibiotic-resistant bacteria that passed screening because tests hadn't specifically looked for that resistance pattern.
This tragedy prompted immediate changes. Donor screening protocols now include comprehensive testing for multidrug-resistant organisms. The FDA issued safety alerts warning that FMT poses particular risks for immunocompromised patients.
Another concern emerged during the mpox outbreak. Unknown pathogens can theoretically transmit through donor stool before screening protocols catch up. This highlights why dynamic screening that adapts to emerging threats matters so much.
Patient selection plays a crucial role in safety. Studies show older patients, those on hemodialysis, and people who require antibiotics immediately after FMT show significantly lower cure rates. Taking antibiotics post-transplant essentially undoes the microbial restoration that FMT provides.

While FDA approval exists only for recurrent C. difficile infection, researchers are exploring FMT for numerous other conditions with promising results.
Ulcerative colitis trials show mixed but encouraging outcomes. Patients with mild-to-moderate disease achieve higher remission induction rates than remission maintenance, suggesting FMT might work better as an acute intervention than a long-term therapy. Meta-analyses of nine randomized trials confirm statistically significant benefits.
Irritable bowel syndrome research demonstrates clear improvements in symptom scores. The CAP-ENEMA trial found that encapsulated FMT produced an 86.7% clinical response rate versus 26.7% for placebo. IBS patients showed increased gut microbiome diversity four weeks post-treatment, with Shannon diversity indices rising from 2.44 to 3.15.
Obesity and metabolic disorders represent an intriguing frontier. Some studies suggest that transferring gut microbiota from lean donors might influence recipient metabolism, though results remain inconsistent. The mechanisms remain poorly understood.
Neurological and psychiatric conditions attract intense research interest because of the gut-brain axis. Early trials exploring FMT for autism, depression, and Parkinson's disease show enough promise to warrant larger studies, though clinical evidence remains preliminary.
For all these experimental uses, the FDA maintains strict enforcement of investigational new drug requirements. Physicians cannot legally perform FMT outside clinical trials except for recurrent C. difficile infection.
"Despite the name, the mechanisms of FMT remain mysterious. Evidence suggests that only spore-forming bacteria or even sterile filtrate may suffice for therapeutic effect, challenging our understanding of what makes the treatment work."
- Krishna Rao, M.D., M.S., American Society for Microbiology
Ideal candidates are patients with recurrent C. difficile infection who have failed standard antibiotic therapy. Clinical guidelines define recurrence as three or more episodes, though some physicians consider FMT after two episodes given its superior efficacy.
Contraindications include severe immunosuppression, particularly patients on high-dose immunosuppressive drugs for organ transplants or cancer treatment. The risk of transmitting opportunistic infections outweighs potential benefits in these populations.
Pregnancy and breastfeeding represent relative contraindications due to lack of safety data. Active inflammatory bowel disease flares, recent gastrointestinal surgery, and suspected intestinal perforation also preclude FMT.
Timing matters significantly. Patients should complete any course of antibiotics for C. diff before receiving FMT, then avoid antibiotics for several weeks afterward to allow the transplanted microbiome to establish itself.
Not all donor-recipient pairings work equally well. Research shows that recipient microbiota profiles converge toward donor signatures after FMT, but the degree of "donorization" varies wildly even among recipients receiving material from the same donor.
This variability suggests that personalized matching - selecting donors whose microbial profile complements a specific recipient's baseline microbiome - could improve outcomes beyond generic donor selection.
Some patients show robust engraftment with lasting symptom relief. Others experience temporary colonization that fades within weeks. Understanding which donor characteristics predict successful, durable engraftment represents a major research priority.
Artificial intelligence tools analyzing donor-recipient compatibility could eventually enable precision matching, similar to organ transplantation matching. The FMTdb database provides exactly the kind of large-scale data needed to train such algorithms.

Pricing for FMT varies dramatically by delivery method and setting. Hospital-based colonoscopic FMT typically costs $1,000-$3,000, mostly for the procedure itself rather than the donor material. Capsule-based treatments run $500-$1,500.
FDA-approved products like Rebyota and Vowst carry manufacturer list prices around $11,000-$17,000 per treatment course, though actual costs vary based on insurance negotiations and patient assistance programs.
Most insurance plans, including Medicare, cover FMT for recurrent C. difficile infection given the strong clinical evidence and American Gastroenterological Association guideline endorsement. Coverage for experimental indications remains limited to clinical trial contexts.
For uninsured patients, the high cost of commercial products creates barriers. Some hospitals maintain donor stool programs to provide more affordable access, though FDA regulatory uncertainty has reduced these programs' prevalence.
The next generation of microbiome therapeutics may not involve human stool at all. Companies are developing defined microbial consortia - specific combinations of cultured bacterial strains that replicate FMT's benefits without the complexity and variability of donor-based transplants.
These synthetic products could offer superior consistency, safety, and scalability. Manufacturers could produce them through industrial fermentation, eliminating donor recruitment and screening costs while ensuring every dose contains identical bacterial composition.
Research into cultured intestinal bacteria and rectal bacteriotherapy suggests this vision is achievable. Several companies have products in late-stage clinical trials.
Rebyota and Vowst represent intermediate steps - standardized formulations from human donors with defined minimum colony-forming units. Rebyota contains at least 1×10^5 CFU of Bacteroides per milliliter and 1×10^8 to 5×10^10 total CFU per milliliter, ensuring consistent microbial load.
True synthetic consortia would take standardization further, using only cultured strains with completely characterized genomes and metabolic functions. This level of control could enable targeting specific metabolic pathways or immune responses.
If you or someone you love struggles with recurrent C. difficile infection that doesn't respond to antibiotics, FMT offers genuine hope with strong evidence backing it. Cure rates above 85% mean most patients achieve lasting relief after one or two treatments.
Talk to a gastroenterologist about whether capsule or colonoscopic delivery makes more sense for your situation. Younger patients without kidney disease generally show better outcomes, but FMT works across age groups.
For other digestive disorders like ulcerative colitis or IBS, the evidence remains mixed. Clinical trials continue, and experimental access exists through research protocols at major medical centers. These conditions may benefit, but they require careful discussion about potential risks versus uncertain benefits.
The rapid evolution from experimental therapy to FDA-approved medicine suggests we're witnessing just the beginning of microbiome-based treatments. As researchers decode how specific bacterial communities influence health beyond the gut - potentially affecting metabolism, immunity, and even brain function - the applications could expand dramatically.
Within a decade, receiving a prescription for beneficial bacteria might become as routine as getting antibiotics. The difference is that instead of killing microbes, we'll be strategically adding them to restore balance.
The ick factor is fading. What remains is remarkably effective medicine that works precisely because it embraces the complex microbial ecosystems we've spent decades trying to eliminate. Sometimes the cure really does come from an unlikely source.
Rotating detonation engines use continuous supersonic explosions to achieve 25% better fuel efficiency than conventional rockets. NASA, the Air Force, and private companies are now testing this breakthrough technology in flight, promising to dramatically reduce space launch costs and enable more ambitious missions.

Triclosan, found in many antibacterial products, is reactivated by gut bacteria and triggers inflammation, contributes to antibiotic resistance, and disrupts hormonal systems - but plain soap and water work just as effectively without the harm.

AI-powered cameras and LED systems are revolutionizing sea turtle conservation by enabling fishing nets to detect and release endangered species in real-time, achieving up to 90% bycatch reduction while maintaining profitable shrimp operations through technology that balances environmental protection with economic viability.

The pratfall effect shows that highly competent people become more likable after making small mistakes, but only if they've already proven their capability. Understanding when vulnerability helps versus hurts can transform how we connect with others.

Leafcutter ants have practiced sustainable agriculture for 50 million years, cultivating fungus crops through specialized worker castes, sophisticated waste management, and mutualistic relationships that offer lessons for human farming systems facing climate challenges.

Gig economy platforms systematically manipulate wage calculations through algorithmic time rounding, silently transferring billions from workers to corporations. While outdated labor laws permit this, European regulations and worker-led audits offer hope for transparency and fair compensation.
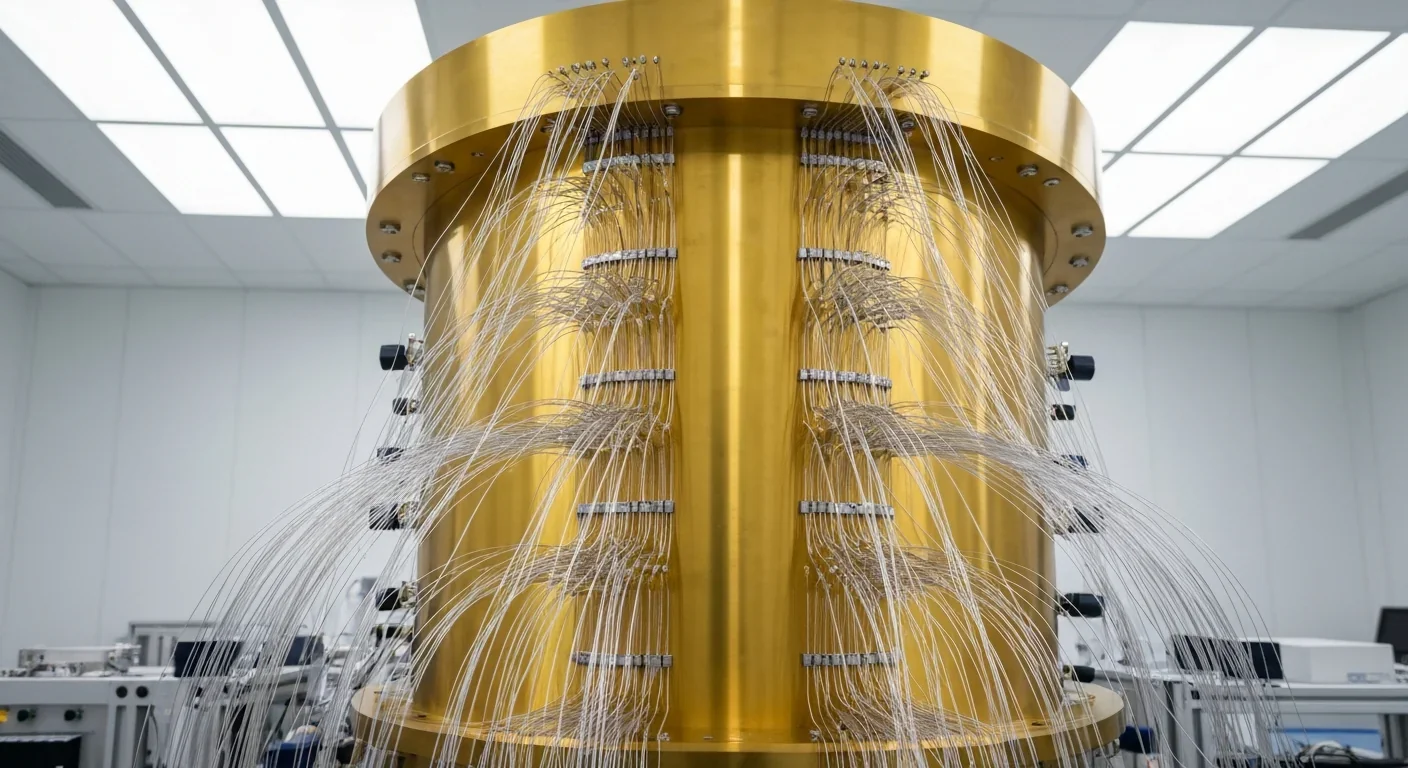
Quantum computers face a critical but overlooked challenge: classical control electronics must operate at 4 Kelvin to manage qubits effectively. This requirement creates engineering problems as complex as the quantum processors themselves, driving innovations in cryogenic semiconductor technology.