The Ancient Protein Clock That Ticks Without DNA

TL;DR: Taking medication at specific times aligned with your circadian rhythm can dramatically improve effectiveness and reduce side effects. Studies show morning cancer immunotherapy extends survival by 13 months, while personalized timing for blood pressure and psychiatric medications optimizes outcomes.

By 2035, your doctor won't just prescribe what medication you need - they'll tell you exactly when to take it, down to the hour. This isn't science fiction. It's chronotherapy, and the evidence is mounting that when you take your pills might matter as much as which pills you take.
A recent multicenter study of 361 cancer patients found something remarkable: those who received immunotherapy infusions before 11:37 AM lived 13 months longer than those treated in the afternoon. The morning group's median survival was 48.4 months versus 35.2 months for evening treatments. That's a 38% improvement in survival, achieved simply by changing appointment times.
We're not talking about a new drug or an expensive procedure. We're talking about using the clock.
Your body runs on a 24-hour cycle, orchestrated by a cluster of about 20,000 neurons in your brain's suprachiasmatic nucleus. This master clock, activated by light signals from your retina, coordinates everything from hormone release to immune cell activity.
But here's what makes this fascinating: nearly every cell in your body has its own clock, ticking away independently. Your liver cells know when you typically eat. Your heart cells anticipate your morning activity surge. Your immune cells ramp up and down on their own schedule.
In 1974, Harvard researcher Charles Czeisler conducted an experiment that would reshape our understanding of human biology. He monitored cortisol levels in volunteers who went to sleep later than usual. The result, in his words, "blew me away." Cortisol levels plunged when people delayed their sleep, proving that timing affects hormone secretion in ways we never suspected.
This isn't just academic curiosity. When Michael Scheer's lab at Harvard simulated night shift work, participants who ate during simulated nighttime hours showed glucose rhythms that shifted by 12 hours. Their post-meal glucose levels spiked higher than people eating the same food during the day. Same calories, same nutrients, dramatically different metabolic response - all because of timing.
The implications for medication are profound. If your body's response to food changes by the hour, why would its response to drugs be any different?
Nowhere is chronotherapy showing more promise than in cancer care. The immune checkpoint inhibitor story is just the beginning.
The research on timing cancer immunotherapy reveals something unexpected: the benefit isn't equal for everyone. Women in the morning treatment group showed a 70% improvement in overall survival. Men? No significant difference. This suggests that chronotherapy isn't a one-size-fits-all solution - it's deeply personalized, potentially influenced by sex hormones that themselves follow circadian patterns.
Prostate cancer radiation therapy tells a more nuanced story. A study of 334 men found that treatment timing didn't significantly affect survival rates, but it did influence side effects. Early morning radiation was associated with modest reductions in urinary incontinence and obstruction. More intriguing: when researchers analyzed the data by race, they found different timing effects in Black versus white patients, hinting at genetic or environmental factors that modify circadian sensitivity.
The molecular mechanisms are becoming clearer. PD-1 and PD-L1 - the immune checkpoint proteins that cancer drugs target - fluctuate throughout the day. So do the populations of immune cells that attack tumors. Cytokine production follows its own rhythm. When you administer an immunotherapy drug during the peak of immune activity, you're essentially amplifying the signal. Give it during the trough, and you're fighting an uphill battle.

For decades, doctors debated whether blood pressure medications work better in the morning or at bedtime. The answer, it turns out, depends on who you ask - and increasingly, on what wearable devices reveal about your personal rhythm.
Blood pressure naturally dips during sleep, then surges in the early morning hours. This "morning surge" is when heart attacks and strokes most commonly occur. The logic seemed simple: take your blood pressure medication at night to control that dangerous dawn spike.
But recent large-scale trials have challenged this assumption. The BedMed-Frail trial, focusing on older adults, found no significant difference in cardiovascular outcomes between morning and evening dosing. What researchers did find was that medication adherence - actually taking your pills - mattered far more than timing.
This creates an interesting paradox. In controlled studies, timing shows clear effects on blood pressure readings. In real-world settings, the benefits get diluted by human behavior. If you're more likely to remember your medication with your morning coffee than on your nighttime routine, chronotherapy becomes irrelevant.
The solution might lie in personalization. Some people are natural "night owls" with delayed circadian rhythms. Others are "morning larks." A 2025 review of chronotherapy in hypertension suggests that matching medication timing to individual chronotypes - rather than using a universal morning or evening schedule - could optimize outcomes while maintaining adherence.
Mental health treatment is entering the chronotherapy conversation, and it's revealing just how intertwined our mood is with our internal clock.
Antidepressants, particularly SSRIs, can affect sleep architecture. Taking them in the morning versus evening doesn't just change when side effects occur - it can influence the drug's effectiveness. Some patients report better mood stability with morning dosing, while others find evening doses reduce anxiety-related insomnia.
The relationship between sleep disorders and psychiatric conditions runs deep. About 80% of people with depression experience sleep disturbances. Circadian rhythm disruption isn't just a symptom - it may be part of the disease mechanism.
Melatonin, the hormone that signals nighttime to your body, has emerged as both a chronotherapy tool and a cautionary tale. Low doses (0.5-5 mg) can help reset circadian rhythms in people with delayed sleep phase disorder. Higher doses often used for "sleep" don't improve circadian alignment - they just act as a sedative. Timing melatonin supplementation wrong can actually worsen your internal clock misalignment.
This highlights a crucial principle: chronotherapy isn't just about taking medications at the "right" time. It's about understanding what "right" means for your biology.
The enthusiasm for chronotherapy sometimes outpaces the evidence, creating pitfalls for both patients and clinicians.
Pitfall 1: Ignoring medication interactions. Shifting one medication to optimize timing can affect how other drugs are absorbed or metabolized. Your morning dose of thyroid medication needs to be taken on an empty stomach, creating constraints on when you can take other morning medications.
Pitfall 2: Confusing correlation with causation. Not every study showing timing effects proves that changing schedules will improve outcomes. The prostate radiation study showed trends toward reduced side effects, but with p-values above 0.05 - interesting, not definitive.
Pitfall 3: Ignoring individual chronotypes. Population-based recommendations (take this drug at 8 AM) ignore that your "8 AM" might be functionally different from someone else's 8 AM. If you naturally wake at 6 AM, your cortisol surge happens earlier than someone who wakes at 9 AM.
Pitfall 4: Sacrificing adherence for optimization. The best medication schedule is the one you'll actually follow. If shifting your blood pressure medication to bedtime means you forget it half the time, you've optimized your way into worse outcomes.
The solution: Start with adherence, then optimize within that constraint. Use medication-tracking apps that prompt you at optimal times. Discuss your daily routine with your healthcare provider so timing recommendations fit your life, not just circadian theory.

The future of chronotherapy isn't just about better timing guidelines - it's about personalization at scale.
Wearable devices are evolving beyond step counting. Modern actigraphy can measure circadian amplitude, phase, and fragmentation in real-world settings. These metrics go beyond asking "did you sleep well?" to quantifying "how synchronized are your rhythms?"
One 2023 study used machine learning on wearable data to predict circadian rhythm health indicators with high accuracy. The algorithm could identify disrupted rhythms that might require intervention, potentially flagging people who would benefit most from chronotherapy before they ever develop symptoms.
The technology is getting more sophisticated. Wearables can now track heart rate variability, skin temperature, and movement patterns - all of which reflect circadian status. When integrated with medication reminders, these devices could theoretically prompt you to take your blood pressure medication not at 8 PM every night, but when your personal cardiovascular rhythm is most receptive.
For clinicians, this creates new possibilities. Imagine reviewing a patient's two-week circadian report before adjusting their medication schedule, rather than relying on a single morning blood pressure reading or a questionnaire about sleep quality.
The challenge is interpretation. Circadian health markers from actigraphy correlate with daytime alertness and metabolic function, but translating those metrics into specific medication timing recommendations requires more research. We're in the phase where we can measure circadian rhythms with increasing precision, but we're still learning what to do with that information.
Despite the growing evidence, chronotherapy hasn't become standard practice. A 2025 editorial in the Journal for ImmunoTherapy of Cancer called chronotherapy "low-hanging fruit" for cancer treatment and issued a call for pragmatic randomized clinical trials.
Why hasn't it happened already? Several reasons. Clinical trials are expensive, and pharmaceutical companies have little financial incentive to study medication timing for off-patent drugs. Oncology scheduling is driven by clinic capacity and patient convenience, not optimal circadian timing. Electronic health records don't easily capture time-of-day medication data, making retrospective analysis difficult.
But the barriers are crumbling. The cancer immunotherapy data is too compelling to ignore - institutions are beginning to preferentially schedule infusions for morning hours. Wearable device adoption is accelerating, creating new data streams. AI algorithms are getting better at personalizing recommendations.
The next decade will likely see chronotherapy move from niche research to mainstream practice, not through a single breakthrough but through accumulated evidence across multiple conditions. Your pharmacist might soon ask not just about drug allergies and other medications, but about your sleep schedule and chronotype.
If you're taking medication for a chronic condition, should you change your timing right now? Probably not without consulting your healthcare provider. But you can start paying attention.
Track when you take your medications and how you feel at different times of day. If you're on cancer treatment, ask your oncologist if morning scheduling is an option. If you take blood pressure medication, discuss whether your current timing aligns with your personal routine and whether adjustment might help.
The bigger message: we're entering an era of precision medicine that isn't just about genetic testing and targeted drugs. It's about recognizing that the human body is a time-based system, not a static machine. The same medication at different times can be a different treatment entirely.
Chronobiology is revealing that one of the most powerful tools in medicine - timing - has been hiding in plain sight. We're not discovering new cures so much as learning to use existing ones with more intelligence. And unlike expensive precision medicine interventions, adjusting the clock on your medications costs nothing.
The future of medicine will be personalized not just to your genes and your disease, but to your rhythms. That future is beginning now, one optimally timed dose at a time.

Ahuna Mons on dwarf planet Ceres is the solar system's only confirmed cryovolcano in the asteroid belt - a mountain made of ice and salt that erupted relatively recently. The discovery reveals that small worlds can retain subsurface oceans and geological activity far longer than expected, expanding the range of potentially habitable environments in our solar system.

Scientists discovered 24-hour protein rhythms in cells without DNA, revealing an ancient timekeeping mechanism that predates gene-based clocks by billions of years and exists across all life.
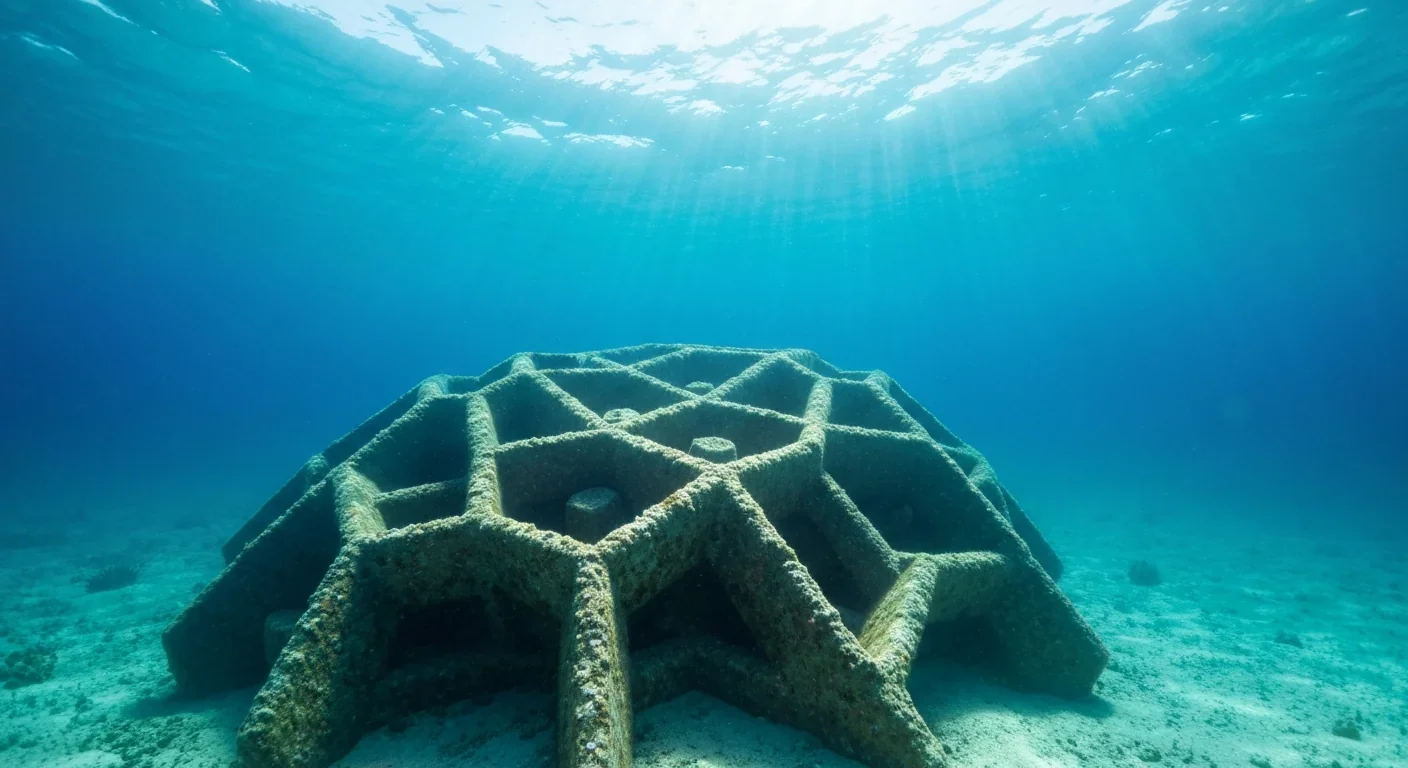
3D-printed coral reefs are being engineered with precise surface textures, material chemistry, and geometric complexity to optimize coral larvae settlement. While early projects show promise - with some designs achieving 80x higher settlement rates - scalability, cost, and the overriding challenge of climate change remain critical obstacles.

The minimal group paradigm shows humans discriminate based on meaningless group labels - like coin flips or shirt colors - revealing that tribalism is hardwired into our brains. Understanding this automatic bias is the first step toward managing it.
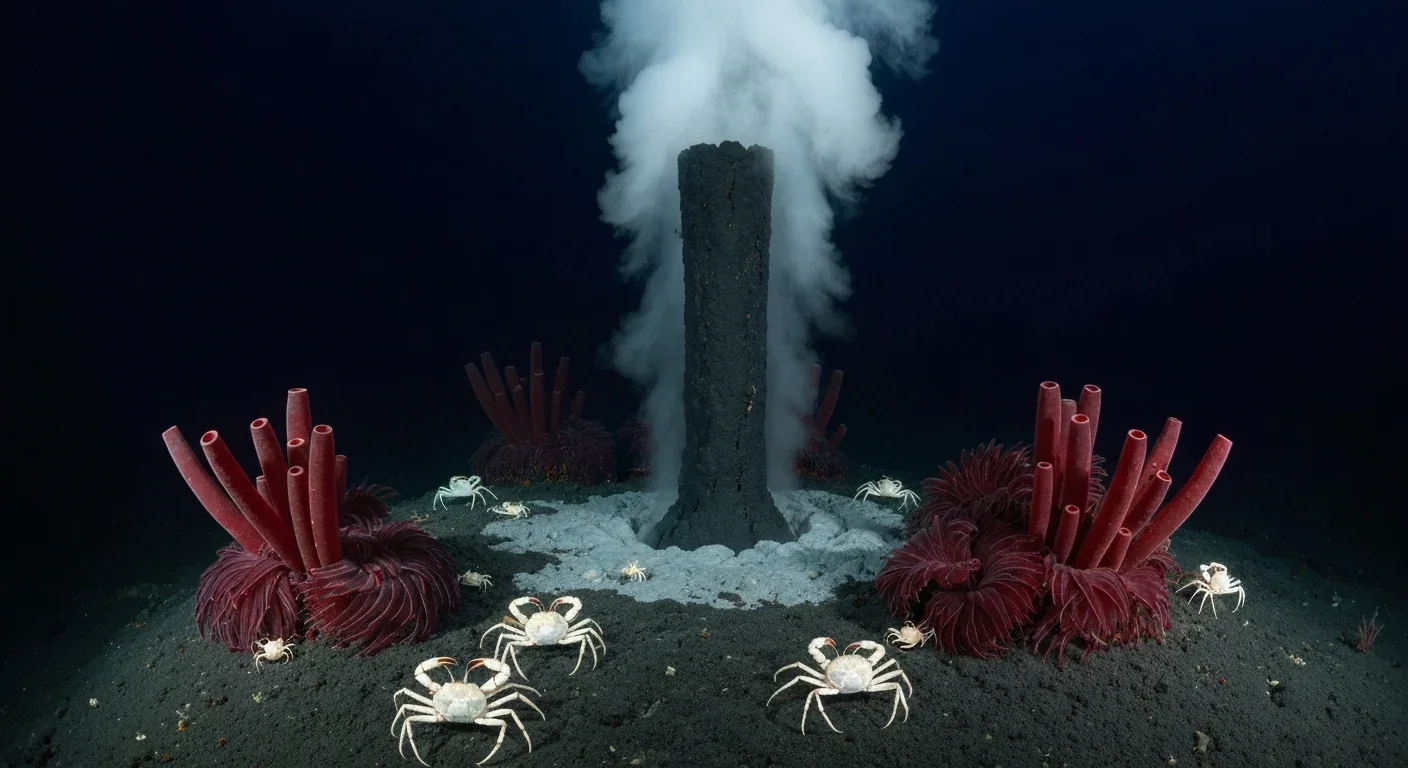
In 1977, scientists discovered thriving ecosystems around underwater volcanic vents powered by chemistry, not sunlight. These alien worlds host bizarre creatures and heat-loving microbes, revolutionizing our understanding of where life can exist on Earth and beyond.

Automated systems in housing - mortgage lending, tenant screening, appraisals, and insurance - systematically discriminate against communities of color by using proxy variables like ZIP codes and credit scores that encode historical racism. While the Fair Housing Act outlawed explicit redlining decades ago, machine learning models trained on biased data reproduce the same patterns at scale. Solutions exist - algorithmic auditing, fairness-aware design, regulatory reform - but require prioritizing equ...
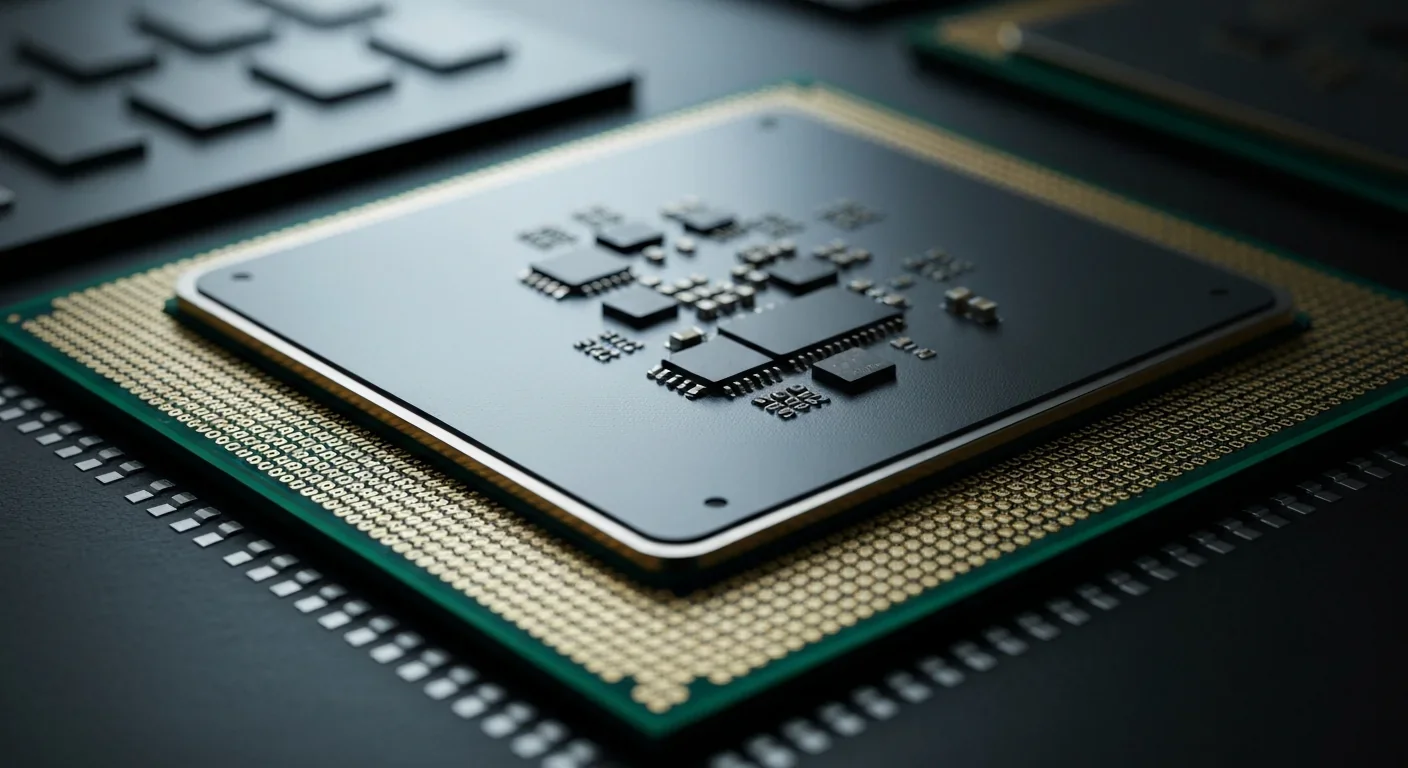
Cache coherence protocols like MESI and MOESI coordinate billions of operations per second to ensure data consistency across multi-core processors. Understanding these invisible hardware mechanisms helps developers write faster parallel code and avoid performance pitfalls.